Eating disorders do not discriminate. Both women and men; younger and older individuals; and all races, ethnicities, and socioeconomic backgrounds are impacted by eating disorders. It is estimated that approximately 20 million women and 10 million men in America will be diagnosed with an eating disorder at some point in their lives. Out of any mental illness, eating disorders have the highest mortality rate. It is not uncommon for an eating disorder to occur with other psychiatric disorders, which is known as co-occuring disorders. With early intervention and effective treatment, recovery from an eating disorder is possible.
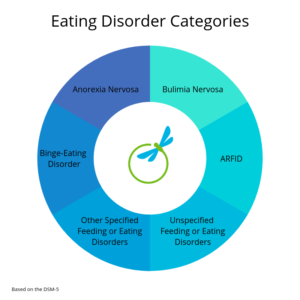
Types of Eating Disorders
Anorexia Nervosa
Anorexia Nervosa is a mental illness characterized by distorted body image, fear of gaining weight, and restricting food and/or compulsively exercising to lower body weight. This illness effects both men and women. It also has one of the highest mortality rates. In a 2011 article published in the Archives of General Psychiatry, at least 1 in 5 anorexia deaths is by suicide. Early intervention is key to successful treatment.
The DSM-5 lists two subtypes of Anorexia Nervosa:
Restricting type: During the last 3 months, the individual has not engaged in recurrent episodes of binge eating or purging behavior (i.e., self-induced vomiting or the misuse of laxatives, diuretics, or enemas). This subtype describes presentations in which weight loss is accomplished primarily through dieting, fasting, and/or excessive exercise.
Binge-eating/purging type: During the last 3 months, the individual has engaged in recurrent episodes of binge eating or purging behavior (i.e., self-induced vomiting or the misuse of laxatives, diuretics, or enemas).
Symptoms:
Physical:
- Extreme weight loss or not making expected developmental weight gains
- Thin appearance
- Abnormal blood counts
- Fatigue
- Insomnia
- Dizziness or fainting
- Bluish discoloration of the fingers
- Hair that thins, breaks or falls out
- Soft, downy hair covering the body
- Absence of menstruation
- Constipation and abdominal pain
- Dry or yellowish skin
- Intolerance of cold
- Irregular heart rhythms
- Low blood pressure
- Dehydration
- Swelling of arms or legs
- Eroded teeth and calluses on the knuckles from induced vomiting
Emotional:
- Severely restricting food intake through dieting or fasting
- Exercising excessively
- Bingeing and self-induced vomiting to get rid of food, which may include the use of laxatives, enemas, diet aids or herbal products
- Preoccupation with food, which sometimes includes cooking elaborate meals for others but not eating them
- Frequently skipping meals or refusing to eat
- Denial of hunger or making excuses for not eating
- Eating only a few certain “safe” foods, usually those low in fat and calories
- Adopting rigid meal or eating rituals, such as spitting food out after chewing
- Not wanting to eat in public
- Lying about how much food has been eaten
- Fear of gaining weight that may include repeated weighing or measuring the body
- Frequent checking in the mirror for perceived flaws
- Complaining about being fat or having parts of the body that are fat
- Covering up in layers of clothing
- Flat mood (lack of emotion)
- Social withdrawal
- Irritability
- Insomnia
- Reduced interest in sex
Bulimia Nervosa
Bulimia Nervosa is an eating disorder characterized by constant preoccupation with weight and body image, resulting in behaviors such as binging and purging, laxative use, excessive exercise, and other means to control caloric intake. Sufferers may be able to maintain their weight for years without anyone around them knowing about their condition. Some of the symptoms of the disorder are:
- Binge eating and eating until painfully full
- Going to the bathroom during or after meals
- Vomiting after meals
- Exercising excessively
- Using laxatives, diuretics or enemas to control weight
- Restricting calories and/or avoiding certain foods between binges
- Mouth sores or sore throat
- Worn tooth enamel
Binge-Eating Disorder
People suffering from Binge Eating Disorder experience recurrent episodes of binging on large quantities of food, followed by unhealthy behaviors to compensate for the binging. During the binge, sufferers experience a loss of control, feeling shame and guilt for the binge episode. People who have this disorder may be of normal weight, but are often overweight or obese. Binge Eating Disorder may result in serious health consequences, including high blood pressure, high cholesterol, diabetes, joint issues, and other conditions. Symptoms are:
- Overeating in a specific period of time, such as two hours
- Feeling out of control when eating
- Eating even when you are full or not hungry
- Rapidly eating
- Eating until you are uncomfortable
- Eating alone or in secret
- Experiencing feelings of shame, disgust, or guilt when eating
- Dieting or participating in other measures to control binge eating
ARFID (Avoidant/Restrictive Food Intake Disorder)
You may have a friend or family member that has a reputation for being a picky eater, but it may be more than just personal preference. Recently added to the DSM-V, ARFID, or Avoidant/Restrictive Food Intake Disorder, is atypical eating or feeding which results in malnutrition, weight loss, and/or emotional distress.
ARFID does impact children and may be more prevalent in individuals diagnosed with autism spectrum disorders. Adults are also impacted by this disorder, too. ARFID may look different for everyone. Some individuals may avoid certain food groups altogether, while others may have a fear of a particular food, or may even be scared of swallowing, choking, nausea, or vomiting.
According to the DSM-5, symptoms of ARFID include:
- An eating or feeding disturbance (e.g., apparent lack of interest in eating or food; avoidance based on the sensory characteristics of food; concern about aversive consequences of eating) as manifested by persistent failure to meet appropriate nutritional and/or energy needs associated with one (or more) of the following:
- Significant weight loss (or failure to achieve expected weight gain or faltering growth in children).
- Significant nutritional deficiency.
- Dependence on enteral feeding or oral nutritional supplements.
- Marked interference with psychosocial functioning.
- The disturbance is not better explained by lack of available food or by an associated culturally sanctioned practice.
- The eating disturbance does not occur exclusively during the course of anorexia nervosa or bulimia nervosa, and there is no evidence of a disturbance in the way in which one’s body weight or shape is experienced.
- The eating disturbance is not attributable to a concurrent medical condition or not better explained by another mental disorder. When the eating disturbance occurs in the context of another condition or disorder, the severity of the eating disturbance exceeds that routinely associated with the condition or disorder and warrants additional clinical attention.
Other Specified Feeding or Eating Disorders
The disorders listed below do not fully meet the criteria of the disorders listed above, but still impact how an individual functions on a daily basis. The DSM-5 lists the following as Other Specified Feeding or Eating Disorders:
- Atypical anorexia nervosa
- Bulimia nervosa (of low frequency and/or limited duration)
- Binge-eating disorder (of low frequency and/or limited duration)
- Purging disorder
- Night eating syndrome
- Unspecified Feeding or Eating Disorders
Unspecified Feeding or Eating Disorder
Resources and Additional Reading:
https://www.allianceforeatingdisorders.com/
https://www.nationaleatingdisorders.org/what-are-eating-disorders
https://www.nationaleatingdisorders.org/warning-signs-and-symptoms
Disordered Eating
Disordered Eating is descriptive of erratic or varied eating patterns that may not be defined by an eating disorder diagnosis. Despite this, the behaviors can be disruptive to a healthful and balanced relationship with food, often consuming significant time and attention.

Symptoms of Disordered Eating:
- Patterns of frequent or yo-yo dieting, eliminating certain foods or meal restriction.
- Chronic weight cycling
- Rules and rigid routines surrounding food and exercise.
- Feelings of regret, fear, guilt and shame around eating.
- Spending time hyper-focused on food, body image and weight.
- Feeling out of control in many situations involving food, which may include restriction, emotional eating or binge eating.
- Using food or exercise in a way to compensate or control food eaten.
Oasis Therapeutic Outpatient Program for Eating Disorders
Given the complex nature of an eating disorder, treatment requires a unified approach from a multi-disciplinary team of professionals. Our entire treatment staff is equipped to deal with not only eating disorders but also with the behaviors, disorders and conditions that often co-exist, including addiction, mood and anxiety disorders, PTSD, trauma, and personality disorders. Our team has specialized training in each of these fields so as to ensure each client the highest level of care. We also have access to a network of Board Certified Psychiatrists and Internal Medicine Specialists who can manage any medical issues if necessary.
Treatment for Eating Disorders at the Oasis is intensive psychotherapy. We are not just focused on symptom management because we believe that if the issues underlying an eating disorder are not fully resolved, relapse is imminent. As such, each client works intensively with an individual therapist in order to explore core beliefs, environmental influences, and emotional drives at the root of the eating disorder. At the Oasis we recognize the complexities of an eating disorder, and understand that treatment is lengthy in nature. We are equipped to address your needs on a long-term basis even after completion of our intensive eating disorder program.
PROGRAM COMPONENTS
Client’s entering the Oasis Program for Eating Disorders can anticipate the following:
- A comprehensive psychological and nutritional intake
- Referral and collaboration with medical and psychiatric professionals
- Personalized psychotherapy and nutritional treatment plan
- Individual nutrition therapy
- Individual, couples and family therapy
- Supportive meal groups in a natural setting
- Intimate and safe group therapies
- Expressive therapies, including dance movement and art therapy
- Dialectical Behavior Therapy (DBT)
- Clinical Enrichment groups and activities
- Weekly clinical case consultation meetings
- Ongoing communication